NSCIBD Investigator Initiated Studies
NSCIBD Program Clinical Database
For future research projects, we would like to have access to a database of patient data that has already been collected. If patients are interested in providing their personal health information to this database, we would collect consent. Signing up to be part of this database is entirely voluntary and refusal to include your information will not affect patient care in any way. Research studies may be conducted using the information contained in the database/registry. Please let our research group know if you would be interested in having your health data copied to our research database.
IBD Strong Peer 2 Peer
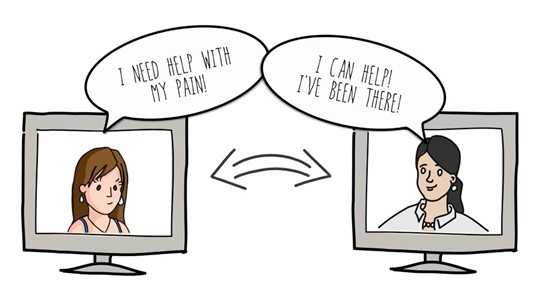
People diagnosed with inflammatory bowel diseases (IBD) endure heightened levels of emotional and mental stress. IBD-associated psychological distress is particularly common at initial diagnosis, during disease flares, before surgery, and during transitions of care. Access to evidence-based psychological interventions and emotional support has been identified as a major care gap by IBD patients. Few patients are asked about psychological distress in routine clinical care and that even if asked, access to mental health care is limited. Despite the clear effect of mental health programs, and the positive effect of social support on self-management and quality of life, there are not many of these programs available. Peer support within healthcare is defined as a person providing emotional and informational support to another person living with a similar chronic illness.
The aim of this study is to improve access to support for mental distress and self-management, through the usage and evaluation of the IBD Strong Peer2Peer program. IBD Strong Peer2Peer is a peer lead program for IBD-related mental distress and self-management.
IBD and Exercise
Research in inflammatory bowel disease (IBD) has shown physical activity to have a positive impact on anxiety, depression, fatigue, and quality of life. However, whether sedentary time (e.g., sitting and watching TV) and physical activity interact to impact these outcomes is unknown for people living with IBD. For example, studies in other chronic diseased populations (lupus, cancer) have shown that replacing 10 to 60 minutes per day of sedentary time with 10 to 60 minutes per day of moderate to vigorous physical activity is associated with better lower body muscular function, less fatigue, and lower blood pressure. Further, people who engage in low levels of sedentary time and high levels of moderate to vigorous physical activity have been shown to have more favorable health outcomes (e.g., better cholesterol) compared to people who have high levels of sedentary time and low levels of moderate to vigorous physical activity.
This study will see if decreasing sedentary time and increasing moderate to vigorous physical activity will impact IBD-related outcomes (e.g., fatigue, quality of life, inflammation).
Biologic Care Pathway
Inflammatory Bowel Disease (IBD) includes Crohn's disease and ulcerative colitis. There are many treatment options for patients suffering from this disease. These options include immune suppressing drugs, surgery, and biologic drugs. Biologics are drugs that are designed to interfere with the patient's immune system in a targeted way. Despite biologic drugs being an important part of IBD care, there is no standard way to use them. Implementing a biologic care pathway (BCP) in clinics could help standardize care and improve treatment outcomes. Research has shown that using a care pathway is a great method to support clinical decision making. It may also improve disease outcomes for patients. This project aims to assess how well a BCP can be blended into clinical practice, improve health outcomes, and reduce healthcare system costs.
The aim of this project is to study the impact of this care pathway on outcomes for patients treated with the help of the standardized BCP compared to those in patients treated without the use of a BCP. The results of this study will inform how best to integrate BCPs into real-world practice.
GUT LINK: A Pilot Study for a Primary Care GI Smartpath
It can be challenging for Primary Healthcare Providers (PHCPs) to differentiate between IBS and more serious illnesses involving the GI tract, such as Crohn’s disease, ulcerative colitis, or cancer. To help with diagnosis and treatment of IBS, evidence-based guidelines have been developed. However, they are not commonly used in primary care practice and PHCPs and patients often feel that GI specialist evaluation and endoscopy is required. Access to specialized GI care in Nova Scotia is limited with patients waiting well beyond published standards to see a gastroenterologist. While the triaging system in the Division of Digestive Care and Endoscopy has helped reallocate limited GI resources where they are most needed, large numbers of patients are excluded from accessing GI specialty care.
The current pilot study is designed to assess the implementation and early comparative effectiveness of a Clinical Care Pathway for lower GI tract symptoms.
the Canadian Network for Virtual Access to Specialists (CaNVAS-IBD) Initiative: A Retrospective Study
Using a virtual nurse navigator introduced in 2022, we plan to see how effective telemedicine can be for IBD patients located in rural areas. The Canadian Network for Virtual Access to Specialists- IBD (CaNVAS-IBD) program was implemented in rural areas of N.S. to offer high quality care organized by an IBD-trained virtual care nurse navigator. This project will compare health outcomes and healthcare resource use of the rural patients who received treatment from the CaNVAS-IBD initiative to patients who received in-person care.
This retrospective chart review study aims to explore the impact of patient navigation in virtual care on health care utilization, quality indicators, and health outcomes of individuals with inflammatory bowel disease (IBD) living outside the major Nova Scotia urban centers.
Assessing stakeholder interest in a virtual dietitian-led Celiac service
The aim of this study is to find the barriers and enablers of providing patient-centered care to people with Celiac disease. A potential strategy is a dietitian-led virtual service. People with Celiac disease referred to the gastroenterology clinic at the QE II Health Sciences Center will be asked to take part in a semi-structured interview. Interview questions will ask about their personal experience in living with Celiac disease and if they received the information and support they needed. We will ask what makes it easier and harder to learn about and follow a gluten free diet. The interview will also ask about celiac knowledge to better learn what they need to learn and the best way to provide this information. We will ask patients and healthcare providers their opinion on a virtual dietitian-led celiac service. We will conduct group interviews with care providers (primary care providers, gastroenterologists, and dietitians) to understand the challenges they face in caring for patients with Celiac disease and how the service could be improved. Based on the what we learn, we will create a dietitian-led celiac service including handouts for patients and processes for healthcare providers to follow.
INTERESTED IN LEARNING MORE ABOUT THESE RESEARCH PROJECTS?
Please contact Natalie Willett (Research Associate) at:
Centre for Clinical Research
5790 University Avenue
Halifax, NS B3H 1V7
Office: 902-473-7074
Fax: 902-473-5889
This email address is being protected from spambots. You need JavaScript enabled to view it.